Hydrogel Could Be Step Forward In Therapies To Generate Bones In Head And Neck
Published in Science Translational Medicine
A team of UCLA School of Dentistry researchers has developed the first adhesive hydrogel specifically to regenerate bone and tissue defects following head and neck surgeries. Their invention was inspired in part by the way that marine mussels can stick to wet surfaces.
Their research is published online in the Journal Science Translational Medicine.
Over the past few years, surgeons and clinicians have begun using hydrogels to administer therapeutic drugs and stem cells to help regenerate lost tissues and bone defects. This approach has advantages over the previous standard treatment, bone grafts, which can lead to inflammation and infection, and which can be costly.
Hydrogels, which are made of networks of polymers, have been found to be effective for carrying drugs and stem cells to targeted spots in the body. But when they’re used during surgeries in the mouth, hydrogels tend to become less effective, because blood and saliva prevent them from properly adhering to a surgical site. As a result, the drugs or stem cells they contain don’t stay in place long enough to deliver their regenerating and therapeutic properties.
“We knew that we needed a product that had optimal adhesion within the confines of the mouth or else our goal to effectively regenerate bone and tissue in the oral cavity would fail,” said Dr. Alireza Moshaverinia, an assistant professor of prosthodontics at the UCLA School of Dentistry and the study’s corresponding author.
Taking inspiration from mussels’ natural ability to adhere to surfaces underwater, the researchers modified their hydrogel by applying an alginate-based solution. Alginates are found in the cells of algae and, when hydrated, form a sticky, gum-like substance.
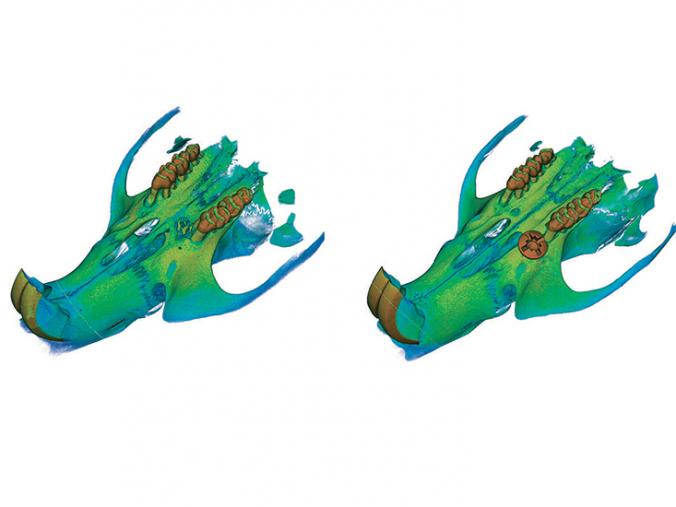
The researchers tested their new hydrogel — loaded with stem cells taken from gum tissue and bone-building bioactive ceramics — in an 18-week study on rats with a version of peri-implantitis, an infectious disease that causes inflammation of the gum and the bone structure around a dental implant.
By the end of the study, the bone around the implants in all of the rats had completely regenerated.
The scientists injected the hydrogel in the mouth and, to seal it in place, applied a light treatment, similar to the method dentists use in humans to solidify dental fillings.
“The light treatment helped harden the hydrogel, providing a more stable vehicle for delivery of the stem cells,” Moshaverinia said. “We believe that our new tissue engineering application could be an optimal option for patients who have lost their hard and soft craniofacial tissues due to trauma, infection or tumors.”
The study’s other authors are Mohammad Mahdi Hasani-Sadrabadi, Patricia Sarrion, Sevda Pouraghaei, Yee Chau, Sahar Ansari, Song Li and Dr. Tara Aghaloo, all of UCLA.
The research was supported by the National Institute of Dental and Craniofacial Research and the California Institute for Regenerative Medicine.
