Deactivating cancer cell gene boosts immunotherapy for head and neck cancers
UCLA discovery opens a pathway toward the discovery more effective treatments
By targeting an enzyme that plays a key role in head and neck cancer cells, researchers from the UCLA School of Dentistry were able to significantly slow the growth and spread of tumors in mice and enhance the effectiveness of an immunotherapy to which these types of cancers often become resistant.
Their findings, published online in the journal Molecular Cell, could help researchers develop more refined approaches to combatting highly invasive head and neck squamous cell cancers, which primarily affect the mouth, nose and throat.
Immunotherapy, which is used as a clinical treatment for various cancers, harnesses the body’s natural defenses to combat disease. Yet some cancers, including head and neck squamous cell carcinomas, don’t respond as well to the therapy as others do. The prognosis for these head and neck cancers is poor, with a high five-year mortality rate, and there is an urgent need for effective treatments.
The UCLA research team, led by distinguished professor Dr. Cun-Yu Wang, chair of oral biology at the dentistry school, demonstrated that by targeting a vulnerability in the cellular process of tumor duplication and immunity, they could affect tumor cells’ response to immunotherapy.
The enzyme they focused on, KDM4A, is what is known as an epigenetic factor — a molecule that regulates gene expression, silencing some genes in cells and activating others. In squamous cell head and neck cancers, overexpression of KDM4A promotes gene expression associated with cancer cell replication and spread.
It is well known that tumor cells can spread undetected by the immune system and, without surveillance, can metastasize to lymph nodes or other parts of the body. In this instance, tumor cells that develop in the epithelial layer that lines the structures of the head and neck can turn into head and neck squamous cell carcinoma when unchecked.
Cancer cell replication occurs through the abnormal spread and activation of signaling pathways for cancer cells, and the researchers asked the question: If we can disrupt these processes and identify a vulnerability, can we change the body’s response to fighting cancer cells and its response to outside immunotherapy?
“We know that the KDM4A gene plays a critical role in cancer cell replication and spread, so we focused our study on removing this gene to see if we would get an opposite response,” said Wang, the study’s corresponding author and a member of the UCLA Jonsson Comprehensive Cancer Center.
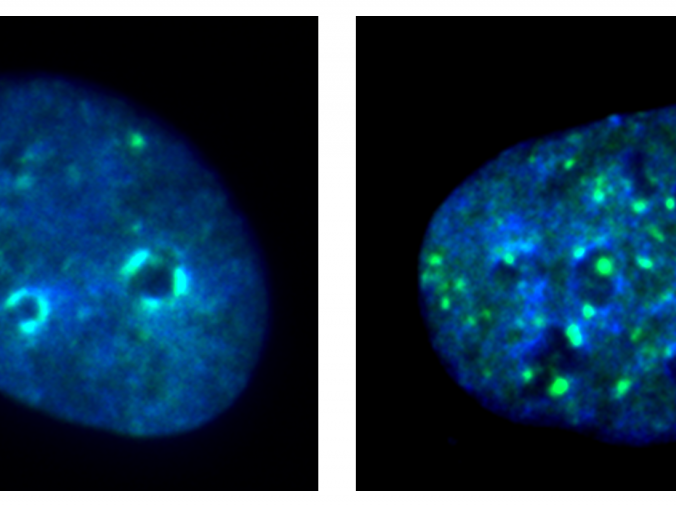
By removing the KDM4A gene in their mouse models, the researchers witnessed a notable decrease in squamous cell carcinomas and far less metastasis of cancer to the lymph nodes — a precursor to the spread of the disease throughout the body. Surprisingly, they also discovered that the KDM4A’s removal also led to the recruitment and activation of the body’s infection-fighting T cells, which killed cancer cells and stimulated inherent tumor immunity.
They then sought to uncover why the squamous carcinoma cells had such a poor response to immunotherapy treatment. In another set of mouse models, they again removed KDM4A and introduced a PD-1 blockade, which signals immunotherapy drugs to attack cancer cells. The combination of immunotherapy and KDM4A removal further decreased squamous cell cancer growth and lymph node metastasis.
Next, the researchers tested whether a small-molecule inhibitor of KDM4A could improve the efficacy of the original PD-1 blockade–based immunotherapy. They found that the inhibitor also significantly helped remove cancer stem cells, which are associated with cancer relapse.
The findings hold promise for the development of more specific inhibitors for KDM4A and more effective cancer immunotherapies.
“I am continuously impressed by Dr. Cun-Yu Wang and his team for breaking through barriers in our understanding of cancer-causing cellular processes,” said Dr. Paul Krebsbach, dean and professor at the UCLA School of Dentistry. “The results of this study have major implications for the development of more effective, life-saving cancer therapies.”
The work was supported by grants from the National Institute of Dental and Craniofacial Research, which is part of the National Institutes of Health.
Dr. Wang is the Dr. No-Hee Park Professor of Dentistry at UCLA, a professor at the UCLA Samueli School of Engineering and a member of Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA.
Additional authors include Wuchang Zhang, Wei Liu, Lingfei Jia, Demeng Chen and Dr. Insoon Chang, all of the Laboratory of Molecular Signaling at the UCLA School of Dentistry and members of the Jonsson Comprehensive Cancer Center, and Dr. Michael Lake and Laurent Bentolila, both of the California NanoSystems Institute at UCLA.
