Bugs as Drugs
Harnessing the therapeutic properties of nisin, an antibacterial peptide, Dr. Yvonne Hernandez-Kapila is making groundbreaking discoveries across oral cancer, periodontal disease, and beyond.
***This story appears in the UCLA School of Dentistry's Spring 2024 Magazine***
If one’s lips are the front door to the human body, then the mouth is its foyer. Exposed to the elements, the condition of each entryway sets the tone for what is found throughout the structure.
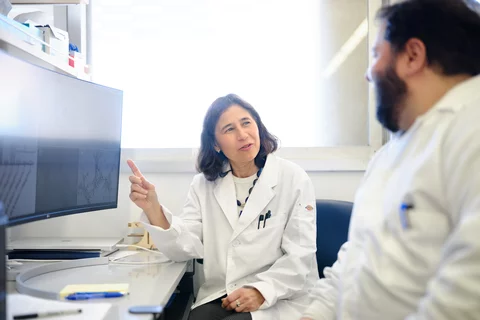
"Although we have a great filtering system in the mouth, it's also very leaky, especially when you have disease,” explained Dr. Yvonne Hernandez-Kapila, the UCLA School of Dentistry’s associate dean of research as well as the Felix and Mildred Yip Endowed Chair. “Gums are very leaky, so that allows an entry point for things outside the body to get into the bloodstream and affect systemic health.”
The gingivae have been central to Dr. Hernandez-Kapila’s career since embarking on a periodontics residency in 1990 at UC San Francisco, also her D.D.S. alma mater. That time period was on the precipice of widespread research into the effect of the oral microbiome – encompassing archaea, bacteria, fungi, and viruses – on the rest of the human body.
Of the four, the oral virome remains the area most ripe for scientific exploration.
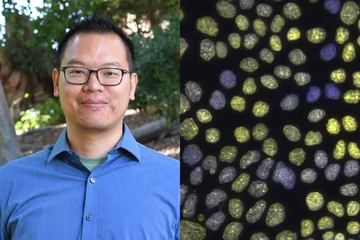
“Viruses are the most abundant species on our planet, and yet we still don't know much about them,” said Dr. Allan Radaic, a project scientist in Dr. Hernandez-Kapila’s lab for seven years who made the move alongside her from UCSF to UCLA in 2022.
Unlike bacteria, which can be cultivated, it wasn’t until recent advances in genome mapping provided an opportunity to investigate the composition of viral communities. Just as important as discovering viruses is identifying potential therapeutics for them.
Leveraging previous findings that individuals with gum disease often develop comorbidities throughout the body, Dr. Hernandez-Kapila knew her research should focus on multimodal treatment; something that could mitigate bacterial growth, inflammation, and cell damage.
Concurrently, the past decade has seen considerable research on the diminishing effectiveness of antibiotics, as bacteria mutate and develop resistance. Pharmaceutical companies have drastically reduced their development budgets in this space – the last entirely original class of antibiotics was discovered in the late 1980s – largely because bringing these drugs to market is often unprofitable. (PMID: 37300874 )
“On top of these two factors, we now know broad-spectrum antibiotics cause collateral damage to other microbes important for human health,” Dr. Hernandez-Kapila said. “Thus, the key to health is not to kill all bacteria, but rather cultivate a balanced microbiota, reaching biosysis.”
Enter nisin.
First identified as a food preservative growing on cheese surfaces in 1928 – coincidentally, the same year penicillin was discovered – over the ensuing century this antibacterial peptide produced by the probiotic Lactococcus lactis has demonstrated a proven safety record, lack of any significant resistance development, and amenability to bioengineering. It was not until the past 20 years, however, that researchers have investigated its therapeutic use. (Nature 586)
“One of the wonderful things about nisin is that it's a very small peptide. It punches holes – if you will – in the membrane of bacteria that allow for ingress of ions that basically kill the bacteria,” Dr. Hernandez-Kapila said.
In 2015, while at the University of Michigan School of Dentistry, Dr. Hernandez-Kapila led the first-ever study into the effects of food-grade nisin on the oral microbiome. Testing different concentrations of nisin on diverse bacteria common to the human oral cavity, this powerful peptide interfered with toxic biofilm development and reduced biofilm thickness. Similarly encouraging, nisin showed no adverse effects on human cells in the oral cavity.
This study was among several authored by Dr. Hernandez-Kapila‘s lab team demonstrating the importance of a balanced microbiota on systemic health … Including its potential to inhibit oral cancers.
“I tried to find money for the longest time to study biosysis, but nobody believed in it. I remember talking to colleagues in the [Michigan] medical school; they're like: ‘This is crazy’,” she said, reflecting on her research journey in the early 2000s. “Then scientific journals and the media started covering the microbiome, and things shifted to: ‘Oh, probiotics, this is so important.’”
In 2022, Dr. Hernandez-Kapila was awarded the largest research grant of her career, for perhaps her most ambitious endeavor to date. A five-year, $5M study funded by the National Cancer Institute (NCI)/National Institutes of Health (NIH) has the potential to make a society-shifting impact:
Our long-term goals are to validate nisin as a promising candidate for oral squamous cell carcinoma (OSCC) treatment and demonstrate that oral dysbiosis is a major driver of tumorigenesis in humans that can be manipulated, thus highlighting the important yet mostly unrecognized protective role that antimicrobials can exert against cancer in humans. (Project report)
Cases of OSCC are increasing despite education about tobacco use and more vaccinations against the Human Papillomavirus (HPV) – two root causes of the disease – and its five-year survival rates have remained unchanged for decades. Dr. Hernandez-Kapila’s exploration of alternative, non-invasive treatment options complements the decade-plus work Dr. David Wong has done in the School’s Center for Oral/Head and Neck Oncology Research to detect cancer at its earliest stages using saliva testing.
“With surgery, radiation, and chemotherapy having such pronounced effects on oral cancer patients, including loss of function and facial deformities, these minimally-invasive diagnostic and therapeutic advancements being made by UCLA Dentistry researchers like Yvonne and David are critical,” said Dean and Professor Dr. Paul H. Krebsbach.
To secure funding, Dr. Hernandez-Kapila leaned on her foundational knowledge as a periodontist and demonstrated irrefutable links between oral pathogens and oral cancer. In 2020, her lab at UC San Francisco induced tumor growth in mice with three such pathogens – T-denticola, P.gingivalis, and F. nucleatum – before rapidly shrinking them with nisin. The control group showed no such abatement. (PMID: 33002094)
This evidence, coupled with a case study in which a human oral cancer patient self-administered nisin and demonstrated improved symptoms, including absence of pain and diminishing tumor size (case study ), helped Dr. Hernandez-Kapila and her co-PI Dr. Sue Yom at UCSF receive FDA approval last year to move forward with Phase I/II clinical trials.
They began in March in Northern California, with subjects ingesting nisin in food or a liquid, milkshake-like form. Data analysis will be conducted by the Hernandez- Kapila Lab team at UCLA.
Researchers hope this new treatment modality will pave the way for the use of antimicrobials as novel therapeutic approaches for multiple forms of cancer beyond the mouth and head and neck, given the known pathways from gingiva to bloodstream.
In preparation for potential FDA approval as an OSCC therapy, Dr. Hernandez-Kapila’s team is concurrently focused on upscaling the power of naturally occurring free nisin for widespread use.
Enter Dr. Radaic, and his expertise working with nanoparticles and nanotechnology.
“My role is to formulate solid lipid nanoparticles loaded with nisin – called SLN-Nisin – in a way that increases the effectiveness in treating diseases, and at lower doses,” Dr. Radaic said of his work, which UCLA holds a patent for.
A native of Brazil, he is one of many diverse researchers to train under Dr. Hernandez-Kapila, from Ann Arbor to Los Angeles to her hometown of San Francisco. As the daughter of working-class immigrants, Dr. Hernandez-Kapila feels a responsibility to expand pathways to increase pathways for the pursuit of scientific knowledge. Among many career honors, Dr. Hernandez-Kapila earned the American Association for Dental Research (AADR) Irwin D. Mandel Distinguished Mentoring Award in 2019.
Diving deep into nisin research has sparked her own curiosity.
“The ‘a-ha’ moments, I think, came, in realizing that nisin has multiple effects,” she reflected. “Not only does it impact cancer cells, but it probably kills bacteria involved in cancer. And it also impacts the inflammation around cancer. I call it multimodal therapy.”
Exploring these numerous modes has led to multiple published findings beyond cancer treatment. Preceding the current focus on thwarting malignant cells was work within her specialty: Periodontal disease.
In a 2020 study (PMID: 35672331), mice were given various experimental treatments, including nisin, to help researchers understand periodontal disease-related alveolar bone loss and inflammation.
Dr. Hernandez-Kapila’s team found that both were mitigated by nisin, while also promoting the number of host reparative cells. This shifting of the oral bacteriome and virome towards a healthy state provided encouraging prospects for human periodontal patients.
Further demonstrating the impact of oral dysbiosis – unbalanced microbiota – on the rest of the body, within the past year the Hernandez-Kapila Lab has authored peer-reviewed journals related to Alzheimer's Disease and gut inflammation
• Nisin, among its other capabilities, has also been found to reduce the number of pathogenic bacteria in the brain, which in turn mitigates the neuroinflammation known as a root cause of Alzheimer's Disease. (J Neuroinflammation 20)
• Periodontopathogens caused lesions in the liver and other organs of the digestive system, establishing the first-ever connection between tooth loss and the progression of liver disease. However, nisin was found to transform the affected microbiomes and serves as a “novel approach to treating NAFLD-steatohepatitis-associated periodontal disease.” (PMID: 38233485)
Dr. Hernandez-Kapila hopes that a successful clinical trial in her NCI-funded study results not only in a widely available oral squamous cell carcinoma therapeutic, but in the quick adoption of nisin-based remedies within each of her focus areas.
“I think once the safety and efficacy are determined, then it will be easier for these other applications to be approved. It sort of creates the right path where the FDA will say: ‘Oh, nisin was already tested safely, so now we want to test it to address fatty liver disease or to address Alzheimer's disease,” she said, optimistically.
Already regarded as the first scientist to connect the brain, gut, and cancer to a healthy oral virome and microbiome, helping bring relief to patients across each of these areas will be a testament to her remarkable career as a researcher.